
1.How did the symptoms develop?
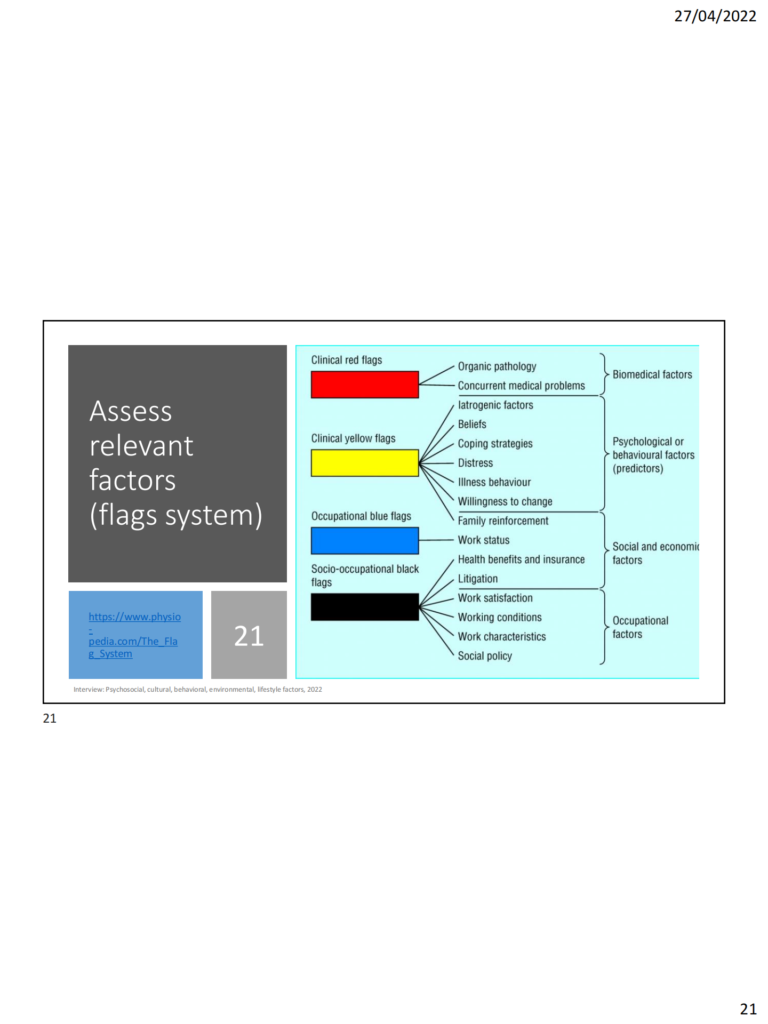
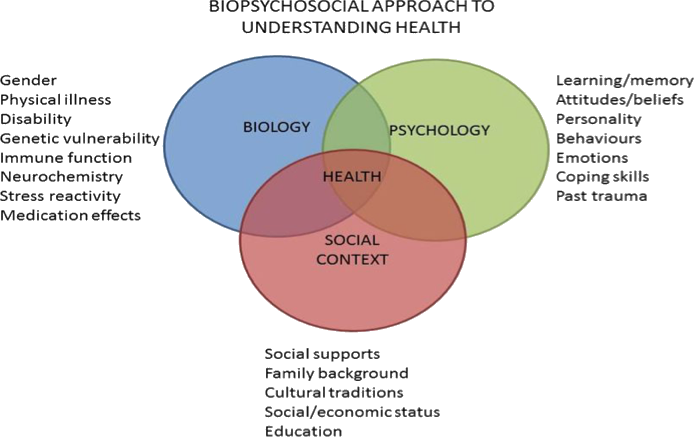
2.What factors might potentially contribute to or maintain the patient’s symptoms?
Work can involve prolonged bent positions. Physical work.
Antidepressant
Family, two kids
“What has brought you here today?
“I see in your notes that you were admitted to hospital last night because you have a chest infection. How are you managing?
• How do you get around at home?
• How do you get in/out of your wheelchair?
• Your GP mentions you have recently had a fall. Can you tell me more about this?
• Can you get up off the ground if you were to fall?
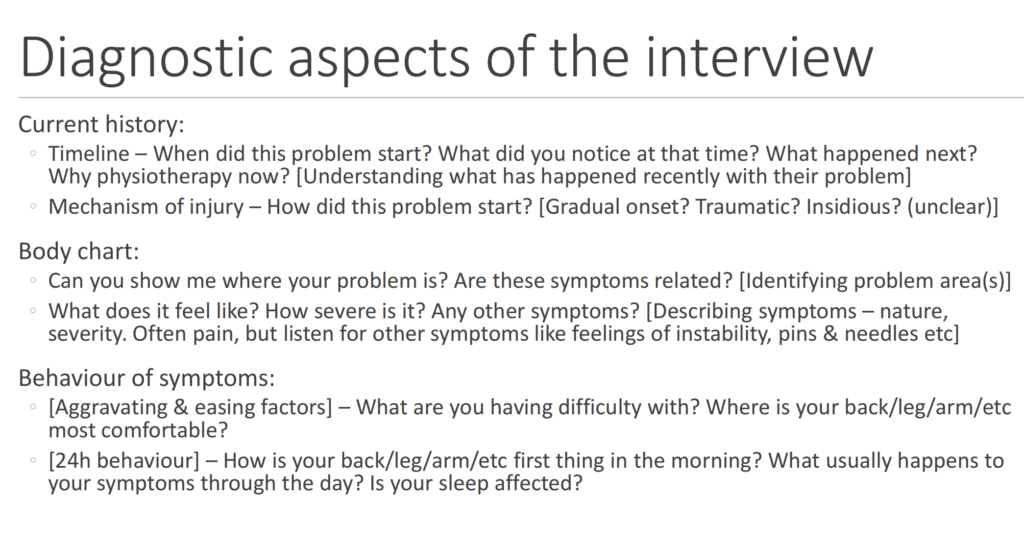
Diagnostic aspects of the interview
Current history:
◦ Timeline – When did this problem start? What did you notice at that time? What happened next?
Why physiotherapy now? [Understanding what has happened recently with their problem]
◦ Mechanism of injury – How did this problem start? [Gradual onset? Traumatic? Insidious? (unclear)]
Body chart:
◦ Can you show me where your problem is? Are these symptoms related? [Identifying problem area(s)]
◦ What does it feel like? How severe is it? Any other symptoms? [Describing symptoms – nature,
severity. Often pain, but listen for other symptoms like feelings of instability, pins & needles etc]
Behaviour of symptoms:
◦ [Aggravating & easing factors] – What are you having difficulty with? Where is your back/leg/arm/etc
most comfortable?
◦ [24h behaviour] – How is your back/leg/arm/etc first thing in the morning? What usually happens to
your symptoms through the day? Is your sleep affected?
Ewan Kennedy April 2022
Contextual aspects of the interview
Social history:
◦ Tell me a bit about yourself. [Who is the person, what is important to them, what activities do they normally
participate in]
◦ How is this problem impacting you? [What is the impact of this problem on the person’s life?]
Past history:
◦ Have you had this problem before? – [Resolved, unresolved, any lessons learnt]
◦ Have you had other problems in this area before? – [any contributors to their current problem]
Special questions
◦ [General health] – Other than your (back pain/sprained ankle etc), how is your general health?
◦ [Medications] – Are you on any medications? (gives insight into health conditions)
◦ [Other health conditions] – Do you have any other health conditions I should be aware of? For example…
◦ [Specific screening questions – region specific, red flags; e.g. Cauda equina syndrome Qs, history of cancer]
Extra for experts
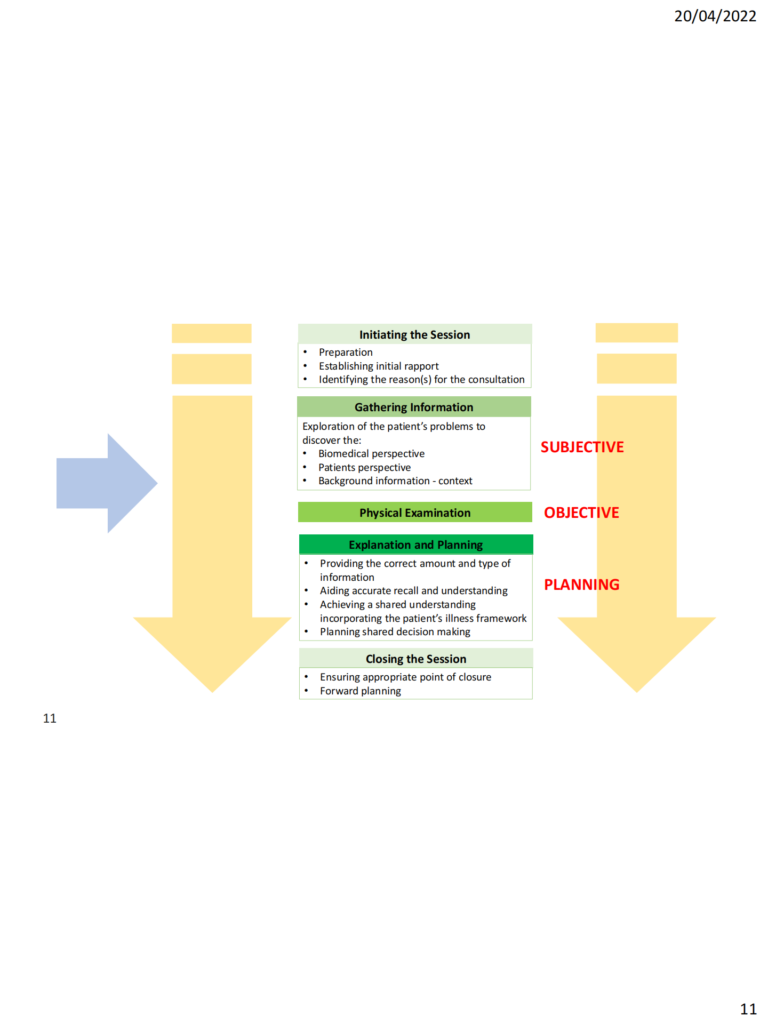
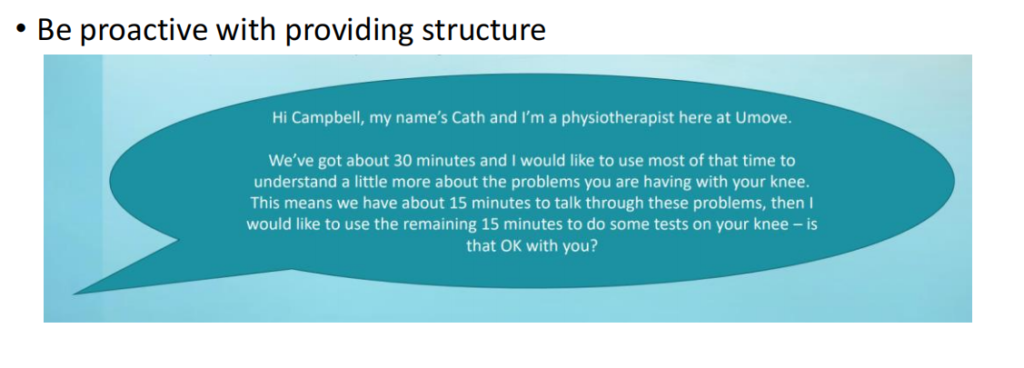
Opening the session well (mostly discussed in other lectures)
◦ E.g. Have you been to physiotherapy before? If not, explaining what the session will look like.
◦ Asking how much time they have
Asking their thoughts about what might be going on
◦ E.g. What do you think has happened?
◦ People are often well informed, googled it, have opinions from friends and family
◦ Right or wrong, their views are valuable
Linking the interview to the physical exam
◦ E.g. It sounds like your quite worried that you’ve broken your finger and from how it happened that’s
certainly possible. Let’s have a good look, move and feel – then we can decide if an x-ray is needed.
◦ Signposting what you’ve figured out so far, and what you need to learn from the exam
And about a million other tips and tricks you’ll pick up in clinical practice – listen and learn.
Keep your eye on the ball
What information should be prioritised?
Main problem (e.g. Low back pain) Current history
Main concern (e.g. Worried it might be serious) Current history
Problem onset (e.g. Gradual) Current history
Type of tissue involved (e.g. Somatic/musculoskeletal, nerve) Body chart
Stage of problem (e.g. Acute) Current history
Process/mechanism of symptoms (e.g. Mechanical, inflammatory) Behaviour of symptoms
Contributing factors (e.g. Anxiety, bending++ at work, overweight) Social, Past, Special Qs
Risk analysis/reasons for caution (e.g. Any red flags) Special Qs, All sections
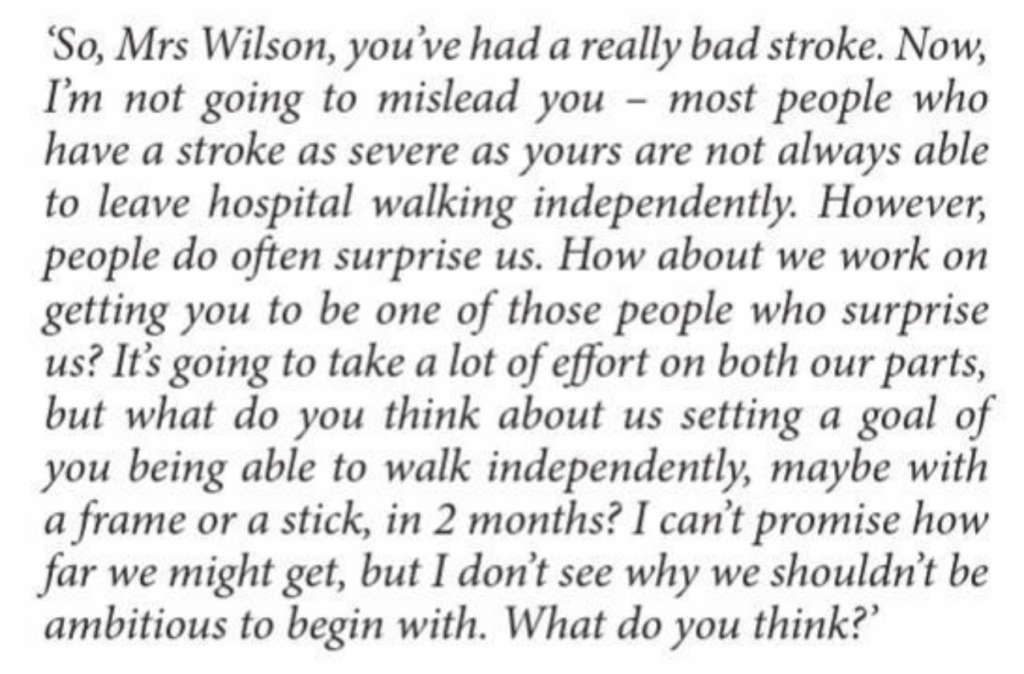
Opening the session
◦ I understand you’ve hurt your knee. Have you been to physiotherapy before?
Interview (full list of questions)
◦ Tell me a bit more about what happened? How did it go? (Clarifying mechanism)
◦ How was the knee immediately afterwards?
◦ Alright so you could put a little bit of weight through it. And any swelling? Current history
◦ How did it go over the next day or so?
◦ What are your main concerns at this point?
◦ And I understand you’re a student, so tell me a bit more about what you get up to normally. Social history
Physical exam
◦ Note signposting what is coming and why (interview skills)
Analysis / discussion with person
◦ Clear links to findings in interview and physical exam
◦ In this case – this discussion directly addresses the main concerns
Management
◦ Initiate MRI referral and some basic early stage rehab – simple and prioritised management
Current History: Initial questions
• Can you tell me about what happened leading up to your hospital
admission?
• How have things changed since you were admitted to hospital?
• What are your main concerns at the moment?
